Researchers identify key biological markers for psychotic disorders
By James Hataway
A team of researchers led by faculty at the University of Georgia has identified a number of biological markers that make it possible to classify mental disorders with greater precision. Their findings, published today in the American Journal of Psychiatry, may one day lead to improved diagnostics and treatments for those suffering from mental illness.
The advent of modern medical diagnostic tools has made it possible to identify the hallmarks of innumerable diseases with simple, reliable tests that portray the inner workings of the body in exquisite detail—allowing doctors to pinpoint the specific cause of a patient’s complaint and prescribe the proper course of treatment.
The same cannot be said, however, for the field of psychiatry. Despite advances in technology, there are no objective medical tests to diagnose mental disorders. Psychiatrists cannot find evidence of schizophrenia in a blood sample; they can’t see bipolar disorder in an X-ray.
“Psychiatry still relies on symptoms as the basis of a diagnosis,” said the study’s lead author Brett Clementz, a professor of psychology in UGA’s Franklin College of Arts and Sciences. “It would be like using the presence of fever to diagnose a specific infection. We need some means to help us more accurately differentiate mental disorders.”
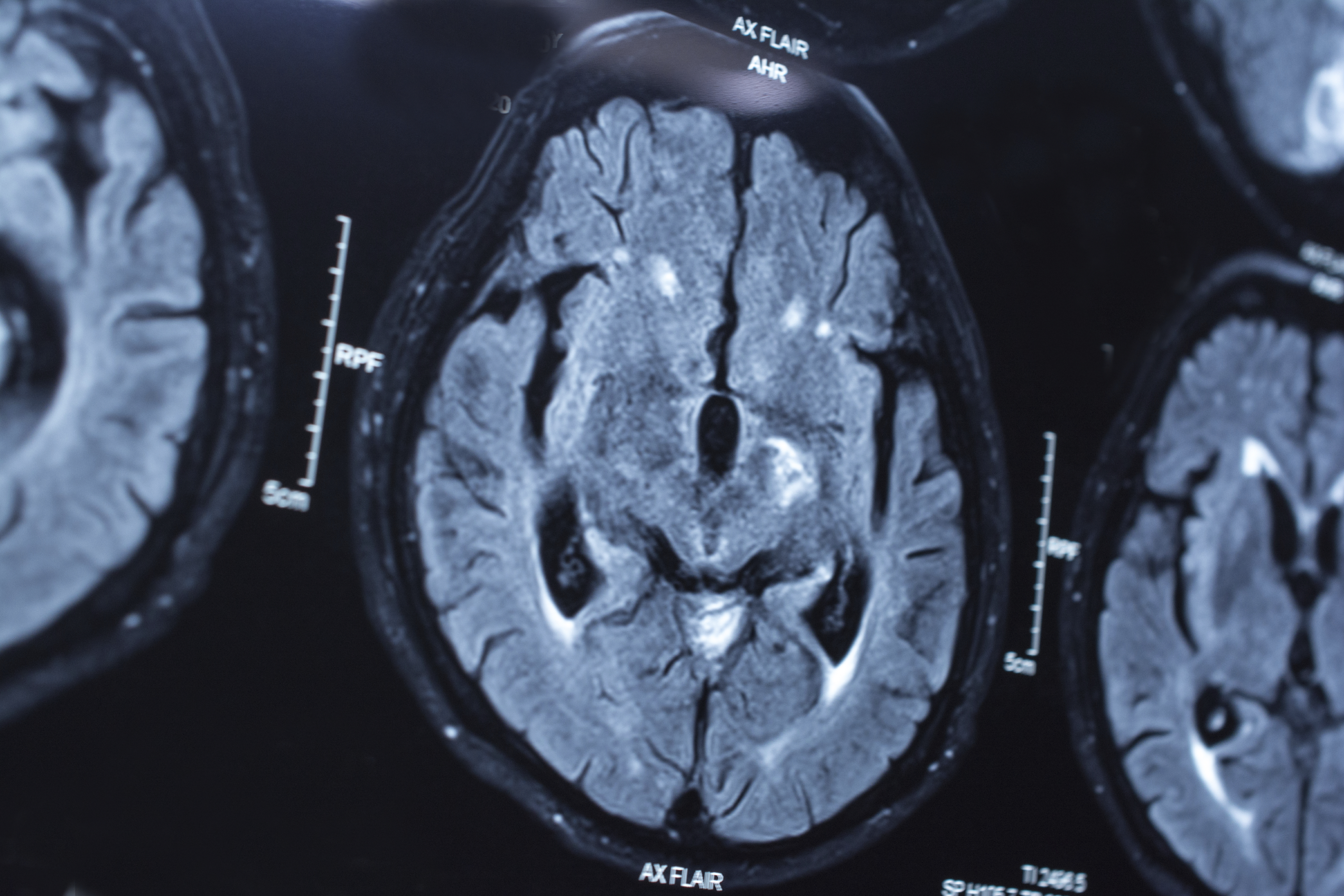
To that end, Clementz and his colleagues created an experimental program that uses neurobiological measures rather than symptoms to identify disease types. They focused exclusively on patients suffering from psychosis—a broad category of mental disorder that includes schizophrenia, schizoaffective disorder and bipolar disorder with psychosis—to see if they could improve upon existing methods.
Mental health professionals traditionally use criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, or DSM, to identify specific mental disorders based on observable symptoms, which, in the case of psychosis, may include hallucinations, delusions, radical changes in personality or a distorted sense of reality.
“We wanted to try to provide neurobiological underpinnings for DSM-type psychosis diagnoses,” Clementz said.
The research team recruited more than 700 patients with psychosis and some of their first-degree relatives—a parent, sibling or child—as well as a control group of healthy individuals to see if they could identify brain-based diagnostic markers to differentiate these conditions.
Each participant went through a battery of tests designed to assess their cognitive abilities, including MRI scans and specially designed examinations that asked participants to respond to simple visual or auditory cues, which reveal sensory and perceptual abnormalities.
Researchers used these measures to identify different “biotypes” of mental disorders, which proved to be superior to DSM standards.
“We were better able to predict who had family histories of psychoses, structural brain abnormalities and measures of social functioning when compared with DSM standards,” Clementz said.
In addition to finding more accurate ways of categorizing disease types, the researchers hope that this project may inspire a renewed interest in psychiatric drug development, which has been stymied recently by a lack of clear biological targets.
“Psychiatry has relied mostly on serendipity for new drugs,” Clementz said. “All of the medications that we use for psychosis have mostly the same mechanism of action, and there are no unique treatments for the various diagnoses.
“You can’t, for example, use an animal model for schizophrenia. How do you find a schizophrenic mouse? But if we can identify a biological mechanism that contributes to disease, then we may reinvigorate drug development, and that’s what we’re trying to provide.”
Clementz is quick to caution that there is still much work to be done before these measures could be used for new diagnostics or to measure drug efficacy, but he is hopeful that this work will lead to much needed advances in the field.
“We’re a long way from identifying specific disease mechanisms, but we’re a step closer than we were when we focused on clinical symptoms alone,” he said.
The project is part of the Bipolar Schizophrenia Network on Intermediate Phenotypes, or BSNIP, a large-scale study designed to discover how risk for schizophrenia and bipolar disorder is transmitted in families and to evaluate risk factors for these diseases.
Research in this news release was supported in part by National Institute of Mental Health grants MH-077851, MH-078113, MH-077945, MH- 077852 and MH-077862.
The study, “Identification of Distinct Psychosis Biotypes Using Brain-Based Biomarkers,” is available at http://ajp.psychiatryonline.org/doi/abs/10.1176/appi.ajp.2015.14091200.